Click Image to View, Download, or Print PDF
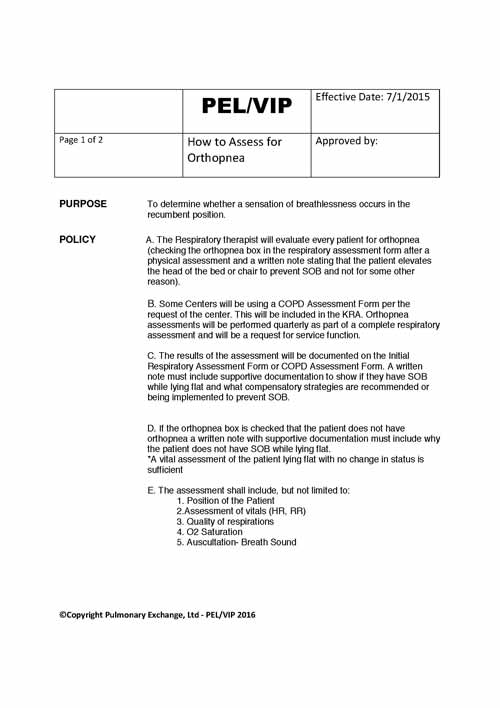
| PEL/VIP | Effective Date: 7/1/2015 | |
| Page 1 of 2 | How to Assess for Orthopnea | Approved by: |
PURPOSE To determine whether a sensation of breathlessness occurs in the recumbent position.
POLICY A. The Respiratory therapist will evaluate every patient for orthopnea (checking the orthopnea box in the respiratory assessment form after a physical assessment and a written note stating that the patient elevates the head of the bed or chair to prevent SOB and not for some other reason).
- Some Centers will be using a COPD Assessment Form per the request of the center. This will be included in the KRA. Orthopnea assessments will be performed quarterly as part of a complete respiratory assessment and will be a request for service function.
- The results of the assessment will be documented on the Initial Respiratory Assessment Form or COPD Assessment Form. A written note must include supportive documentation to show if they have SOB while lying flat and what compensatory strategies are recommended or being implemented to prevent SOB.
- If the orthopnea box is checked that the patient does not have orthopnea a written note with supportive documentation must include why the patient does not have SOB while lying flat.
*A vital assessment of the patient lying flat with no change in status is sufficient
- The assessment shall include, but not limited to:
- Position of the Patient 2.Assessment of vitals (HR, RR)
- Quality of respirations
- O2 Saturation
- Auscultation- Breath Sound
PROCEDURE A. VERBAL– during the Initial assessment of the patient:
- Verbally ask the patient if they become short of breath when lying flat
- If they answer “yes” ask them how do they reduce their SOB (pillows, bed elevation, lay on one side, sleep in chair etc.)
- Determine sleeping position that patient uses to eliminate SOB (number of pillows, head of bead elevation, chair position etc)
- Document patient strategies
- If the patient answers “no” to SOB while lying flat ask them if you can lower the bed (or chair if it reclines) and perform a vital sign assessment and compare it to the initial assessment to compare any change in condition
- Document Findings
- PHYSICAL– during the Initial assessment of the patient:
- Obtain initial patient vitals signs (include patient position)
- Lay the patient to a high fowlers’ position if patient is able and obtain vital signs
- if patient tolerates position lower patient to standard fowlers’ position and obtain vital signs
- If patient tolerates position repeat process to semi-fowlers’ position and obtain vital signs
- If patient tolerates position repeat process to low-fowlers’ position and obtain vital signs
- If patient tolerates position repeat process to supine position and obtain vital signs
- Stop procedure if vital signs increase of SOB occurs or if patient requests termination.
- Document results and reason and position of physical assessment
Use words such as Supine, Fowlers, High Fowlers, Semi Fowlers
-
-
- Fowler’s Position
- A person in the Fowler’s position is sitting straight up or leaning slightly back. Their legs may either be straight or bent.
- A ‘high fowlers’ position is someone who is sitting upright. (A 90 degree angle)
- A ‘standard fowlers’ position is someone at a slight angle. (45-60 degrees)
- Fowler’s Position
-
iii. A ‘semi fowlers’ position is someone whose head is in a semi upright position. (30-45 degrees)
iii. A ‘low fowlers’ position is someone whose head is only slightly elevated. (15-30 degrees)
CONSIDERATIONS
- Be sure to always monitor your patients’ saturations, heart rate, breath sounds while performing this method
- Increase or decrease in RR, HR or Oxygen saturation
- The following signs may indicate a respiratory problem:
-
-
- Irregular pulse
-
- Document on Initial respiratory assessment form.
- Check “Orthopnea box” yes or no on Initial respiratory assessment and document a written note under respiratory evaluations and/or notes/observations and a strategy under recommendations
b.
- If the PHYSICAL method was used, document what position relieved patients’ shortness of breath.
- Document tolerance of procedure as well
1. Monitor non-verbal patients by performing vitals, but also look for signs of intolerance such as shortness of breath and restlessness.
CONTRAINDICATIONS
- Inability to lie flat
- Lightheadedness or dizziness
- Respiratory distress
- Vomiting
- High risk for aspiration
- Lethargy